Fungal dysbiosis following antibacterial monotherapy in canine otitis externa
12 December 2024
Ross Bond and collaborators Jonna Juhola, Erin Brennan, Ewan Ferguson, Anette Loeffler, Anke Hendricks and Sian-Marie Frosini from the Royal Veterinary College, University of London have been awarded BSAVA PetSavers funding to study fungal dysbiosis following potent antibacterial monotherapy in canine otitis externa.
Introduction
Ear disease accounts for around 10% of cases seen in canine practice. Secondary infections with bacteria or Malassezia yeasts commonly exacerbate the clinical signs and complicate the treatment. Drug-resistant bacteria, such as Pseudomonas spp., are especially challenging to treat, particularly if the infection extends to the middle ear. Conventional licensed ear-drops may be ineffective and are contra-indicated if the ear drum is ruptured because of the risk of damage to delicate neural tissues deep within the ear.
In such cases, dilutions of injectable formulations of highly-efficacious antibiotics (often fluoro-quinolones or synergised extended spectrum penicillins) are applied directly into the ear because of their high activity against difficult pathogens, and their enhanced safety when the ear drum is ruptured. These drugs can be prescribed only with owner consent under the ‘prescribing cascade’ when conventional products fail, and/or because there are no drugs licensed for use in canine middle ear infections.
Whilst this approach is commonly effective in treating the original multidrug-resistant bacterial infection, we have observed by cytological examination that Malassezia yeast overgrowth is a not-infrequent sequel. The healthy canine ear canal is normally colonised by a harmonious mixture of bacteria and Malassezia. ‘Dysbiosis’ refers to the condition of imbalance in the microbial communities either in or on the body; whilst this term is perhaps most familiar in the context of the intestinal microbiome, it is equally applicable to microbial disturbances in the cutaneous ecosystem. We hypothesised that removal of bacterial competitors within that ecosystem allows yeasts to multiply and create a new infection, likely favoured by various predisposing, primary and perpetuating factors that facilitated the original bacterial infection. Since this phenomenon is not well-described in the literature, we prospectively studied changes in ear microbes during treatment using quantitative microbiological techniques.
Demonstration of regular Malassezia infection would alert clinicians for the need to monitor for this, and to consider preventative antifungal therapy.
What are the aims of this study?
The primary aim was to quantify Malassezia populations in the ear before and after antibacterial monotherapy to determine whether yeast populations increase in response to successful antibiosis. Should the hypothesis that populations opportunistically increase when highly efficacious broad-spectrum antibiotics remove commensal and infecting bacteria be confirmed, this would alert clinicians to the need to monitor closely for the development of yeast infection in these circumstances. A secondary aim was to quantitatively assess the antibacterial efficacy of the topical antibiotics used.
What have we learned so far?
Preliminary results were presented as a poster at the 34th European Veterinary Dermatology Congress organised by ESVD-ECVD at Gothenburg in August 2023.
Twenty-five dogs with bacterial otitis were treated topically with either fluoro-quinolone (0.5% enrofloxacin [14 dogs, 19 ears] or 0.2% marbofloxacin [one dog, one ear]), with 0.1% dexamethasone)(ʻFQʼ) SID, or 225 mg/mL piperacillin / 25 mg/mL tazobactam (ʻPTʼ) BID (10 dogs plus two FQ failures, 17 ears) for 8–32 d (median 20 d). At Visit 1 and Visit 2, ear swab tips were washed in PBS+Triton X-100 and dilutions spread-plated onto blood, MacConkey (37°C, 48 h) and mDixon’s agar (32°C, 14 d). Microbes were identified by phenotype and matrix-assisted laser desorption ionization time-of-flight spectroscopy.
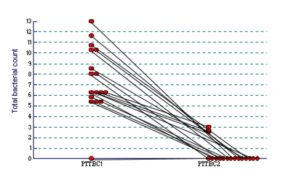
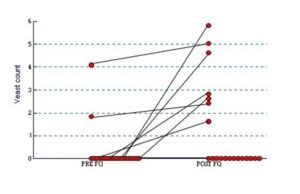
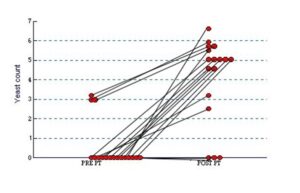
Pseudomonas aeruginosa was the most frequently isolated bacterium at the first visit, followed by staphylococci, streptococci and enterococci. P. aeruginosa was absent post-treatment in 4/8 fluoroquinolone-treated dogs (6/11 ears) and 9/11 piperacillin-tazobactam treated dogs (13/16 ears). Piperacillin-tazobactam treatment resolved pseudomonad infection in two dogs (three ears) that persisted despite fluoroquinolone treatment. M. pachydermatis was isolated in low counts at V1 in two FQ and two PT-treated dogs (two and three ears, respectively), and after treatment in six FQ-treated and 11 PT-dogs (seven and 15 ears); two dogs (three ears) yielded Candida post-treatment. Initial bacterial counts (median log10[CFU/swab+1], lower-upper quartile) (FQ: 6.58, 2.87–9.83; PT: 6.66, 6.06–10.28) were significantly (P<0.001, Wilcoxon) reduced at V2 in both treatment groups (FQ: 0, 0–5.34; PT 0, 0–0) (Fig. 1a and 1b). Overall, initial M. pachydermatis counts (FQ: 0, 0–0; PT: 0, 0–0) were significantly (FQ, P=0.018; PT, P<0.001) increased post-treatment in both groups (FQ: 0, 0-2.55; PT 5.11, 3.38–5.68) (Fig. 2a and 2b).
What will be the benefits of this research?
The preliminary findings confirm our hypothesis, based on previous cytological assessments, that potent antibacterial monotherapy in canine otitis externa/media promotes overgrowth by Malassezia pachydermatis. The observation of Candida overgrowth in two dogs was a novel and unexpected finding. These data provide further evidence that the cutaneous mycobiota is part of a dynamic and interactive cutaneous ecosystem that responds to varied intrinsic and extrinsic factors, such as skin disease and topical therapy. It is envisaged that further recruitment of study dogs will support and strengthen these preliminary findings.
Topically-applied piperacillin-tazobactam was highly efficacious in treating Pseudomonas otitis externa, although subsequent M. pachydermatis overgrowth has been especially frequent. [Colleagues practicing in the European Union should be aware that use of this drug in animals is now prohibited by European law]. These findings indicate the need for future prospective studies to identify measures that will prevent fungal dysbiosis, perhaps by concurrent use of antiseptic ear rinses or prophylactic antifungal drugs. A proactive, or preventative approach will thus provide an opportunity to enhance patient welfare by limiting ongoing ear disease.
Colleagues in both specialist and primary care veterinary practice should be aware that cases that respond favourably to antibacterial monotherapy must be monitored for yeast overgrowth.
Thinking of applying for BSAVA PetSavers funding?
The authors are most grateful to BSAVA PetSavers for funding this study which enabled us to confirm our previous cytological observations. It was most gratifying to be able to clearly demonstrate the phenomenon of fungal dysbiosis in canine otitis externa and to provide justification for future investigations aimed at prevention. It is difficult to obtain funding for small clinical studies of relevance to daily clinical practice, and in this regard BSAVA PetSavers is an ideal point of contact for that support.
About the author
Supporting more BSAVA PetSavers research
BSAVA PetSavers is supported solely by charitable donations. Help fund more clinically-relevant veterinary research by donating today at www.bsava.com/petsavers/donate.